Our history is a battle against the microbes: we lost terribly before science, public health, and vaccines allowed us to protect ourselves
For most of our history, we were losing terribly against the microbes. Only recently did we turn the battle in our favor. Vaccines were a major breakthrough.
For most of our history, we were losing terribly against the microbes. Only recently did we turn the battle in our favor. Vaccines were a major breakthrough.
Humanity’s history is a continuous battle between us and the microbes.1 For most of our history, we were on the losing side.
It wasn’t even close. We were losing very decisively. Billions of children died from infectious diseases. They were the main reason why child mortality was so high: No matter where or when they were born, around half died as children. We looked at the evidence of child mortality in pre-modern times here.
The recurring epidemics of influenza, measles, cholera, diphtheria, the bubonic plague, and smallpox also killed large parts of the adult population. Within just a few years, the Black Death killed half of Europe’s population.2 The epidemics – especially of smallpox, but also measles, typhus, and other diseases – that the colonialists brought from Europe with them to the Americas often killed an even larger share of the population.3
The world today is very different. Infectious diseases are the cause of fewer than 1-in-6 deaths, and as the world made progress against the microbes, our lives became much longer. The global average life expectancy is now 73 years after life expectancy doubled in every world region.
Until recently, no one knew where diseases came from
How is it possible that for millennia we were losing the battle against the microbes so awfully and then turned things around in just a few generations?
Science is the foundation for our success. 150 years ago, nobody knew where diseases came from. Or, more precisely, people thought they knew, but they were wrong. The widely accepted idea at the time was the “miasma” theory of disease. Miasma, the theory held, was a form of "bad air" that causes disease. The word malaria is a testament to the idea that ‘mal aria’ – ‘bad air’ in medieval Italian – is the cause of the disease.
Thanks to the work of a number of doctors and chemists in the second half of the 19th century, humanity learned that not noxious air but specific germs cause infectious diseases. The germ theory of disease was the breakthrough in the fight against the microbe. Scientists identified the pathogens that cause the different diseases and thereby laid the foundation for perhaps the most important technical innovation in our fight against them: vaccines.
Vaccines get your immune system ready for the battle
Vaccines protect us from infectious diseases by offering our bodies a training session on fighting the germs that cause the disease. “The fundamental idea of a vaccine is deliberate exposure to a relatively harmless or dead version of a germ. The immune system will then recognize and eliminate that germ rapidly if it is encountered again,” as vaccine developer Richard Moxon says.4
The trick is that the ineffective form of the pathogen is not causing the disease but resembles the effective pathogen so much that it triggers our body’s natural immune system to produce the antibodies that destroy that pathogen. The training session it provides to the body means our immune system will recognize the invader once we become infected with the real pathogen later in life. Our immune system can quickly muster up what it learned from the vaccine response and immediately start fighting the pathogen.
Public health: You are only safe if everyone else is safe
Vaccines not only protect the health of the immunized person but also the health of the community. If vaccination rates are high enough, the transmission of infectious diseases is interrupted in the community, which means that even those who are unvaccinated gain protection.
As is often the case in development, you cannot achieve progress alone. Your progress toward a healthier life depends on everyone else’s progress toward a healthier life; you’re safer if others are vaccinated too. The health improvements that you cannot achieve by yourself in public health, and many of the most important interventions in the fight against infectious diseases, were therefore financed socially. Public spending financed the crucial improvements in sanitation and many large vaccination programs.
Vaccination programs are one of many strategies by which we made progress against infectious diseases. The first pathogen successively defeated by humans in Europe – as early as the 17th century – was the plague. According to Shaw-Taylor (2020) this was achieved by combining quarantine measures, cordons sanitaire, and contact tracing (first developed in the Renaissance).5
Since then, we have found many additional strategies against the various microbes. Antibiotics, safe drinking water, better housing, better education, falling poverty, declining undernourishment, pasteurization, hygiene, better sanitation, and other public health advancements were and are crucial. Jason Crawford provides an excellent overview of the crucial role of better sanitation, hygiene, and other public health measures for progress since the 19th century.
Today too, vaccines are only one of many strategies that we have found in the battle against microbes. We see now – in the COVID-19 pandemic – that there are several countries responding successfully to the virus without the help of a vaccine (we studied how they do this here).
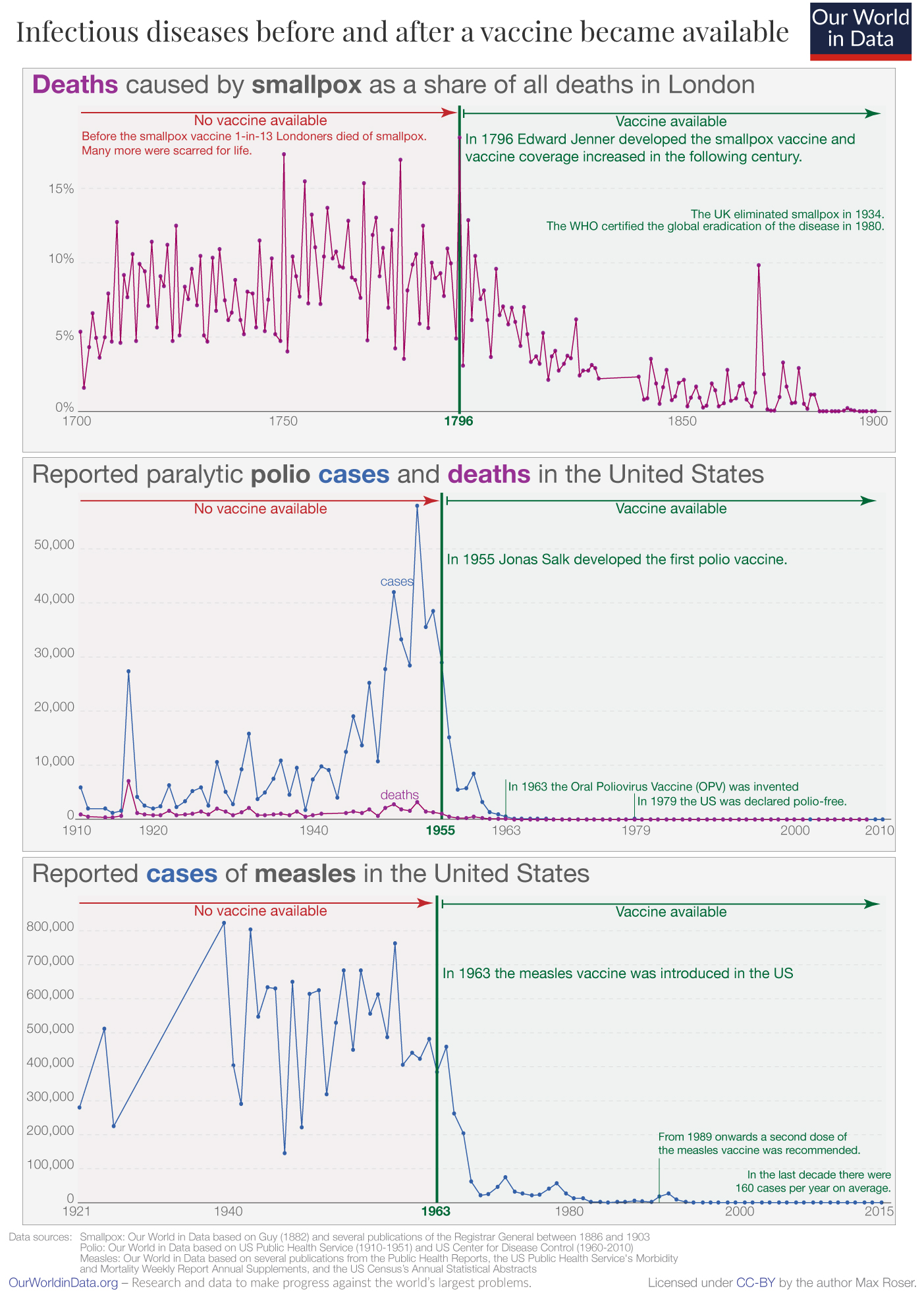
Infectious diseases before and after the vaccine was introduced
How effective were these training sessions against infectious diseases?
In the three charts, I plotted the evolution of three infectious diseases over several decades. You see the data before and after the first vaccination became available.
Smallpox was one of the worst killers in our history. Epidemiologist Donald Henderson suggests that in the last hundred years of its existence, smallpox killed at least half a billion people.6 Even more people were disfigured by the disease for the rest of their lives.7 Despite all efforts, humanity never found an effective treatment. But we invented something even better: a vaccine, the very first vaccine ever.
In England in the mid‐eighteenth century, it was probably the leading cause of death.8 But in the following century – as the vaccine reached more people and improved over time – it became rarer and rarer as a cause of death.
Eventually, the disease was eliminated in entire countries, then entire continents, and today, the disease does not exist anywhere in the world. The smallpox vaccine made it possible to completely eradicate the disease. Its eradication has saved the lives of around 150 to 200 million people since.
Our research and data on smallpox
We eradicated one of the worst infectious diseases globally.
The history of polio is similar but more recent. Polio epidemics spread panic at a time that many today can still remember. Polio is an infectious disease contracted predominantly by children that can lead to the permanent paralysis of various body parts. Ultimately it can cause death by immobilizing the patient’s breathing muscles.
The chart shows data from the US, where the first vaccine was developed and used. In the first half of the last century, the US suffered large outbreaks, with many tens of thousands paralyzed. Patients’ only chance to survive was to be confined to a large, mechanical breathing apparatus: the so-called ‘iron lungs’.
The recurring outbreaks ended in 1955 when Jonas Salk developed the polio vaccine. When it was announced on April 12, it was celebrated as “more than a scientific achievement”, according to Salk’s biographer Richard Carter.9 The vaccine, he writes, “was a folk victory, an occasion for pride and jubilation… people observed moments of silence, rang bells, honked horns, blew factory whistles, fired salutes,… took the rest of the day off, closed their schools or convoked fervid assemblies therein, drank toasts, hugged children, attended church, smiled at strangers, and forgave enemies.”
As the chart shows, these celebrations were not misplaced. Over the coming years, vaccination campaigns reached many American children, and the terrible epidemics ended. By 1979, the US was declared polio-free.
Today, our generation has the chance to achieve for polio what has been achieved for smallpox: eradicate it completely. Thanks to the vaccine, humanity has made massive progress towards this goal. In the early 1980s, there were between three- and four-hundred-thousand paralytic cases every year. In the last 12 months (as of the time of writing), there were 298 polio cases globally.10
Our research and data on polio.
With the help of the vaccine, we might be able to eradicate polio globally.
Measles, too, was a major killer for many centuries. The WHO reports: “Before the introduction of the measles vaccine in 1963 and widespread vaccination, major epidemics occurred approximately every 2–3 years, and measles caused an estimated 2.6 million deaths each year.”11
Measles is both very deadly and extremely contagious. Published estimates of the basic reproduction number (R0) – the average number of secondary cases arising from each case – range from 3.7 up to 203.12
The chart shows how rapidly we made progress against this killer after the invention of the vaccine. Once it was introduced in the US, the large outbreaks of the airborne disease ended. The measles vaccine, too, changed world history and the history of millions of families.
Globally we have also made a lot of progress. Today, 85% of one-year-olds receive the measles vaccine, and the number of deaths has fallen from 2.6 million to 83,000 in the latest data.
Smallpox, polio, and measles are just three of the diseases we have vaccines for. We now have effective vaccines against at least 28 diseases.13
I selected these three diseases because they protect us from particularly terrible diseases. The vaccines for polio and measles stand out because even the very early-stage prototypes were very efficacious; the efficacy of many other vaccines increased slowly over time as researchers made adjustments that improved them.
Science is our best strategy now
Some of the best training you ever received were the vaccines you were given in early childhood. Without even realizing it, you learned how to battle the pathogens that ravaged the lives of your ancestors for many millennia.
When humanity achieves very substantial progress, it can become difficult to understand what the problems were that we made progress against. This is also the case for vaccine-preventable diseases. Infectious diseases that once disfigured, pained, paralyzed, and killed many of our ancestors have disappeared so far from our lives and memories that some today can afford the luxury of disregarding or even avoiding vaccination.
Today, as we face the COVID-19 pandemic, many of us experience for the first time with one infectious disease, what our ancestors experienced with a whole range of them. Just as they were without protection against the diseases discussed previously, we are now facing a pathogen that we have no treatment for and no protection from.
And now, just as back then, our best hope is science. The responses from South Korea, Vietnam, and Germany show that it is possible to fight the disease successfully, but to end the suffering COVID-19 causes, our best hope is a vaccine against it.
We were never better equipped to battle a virus. The genome was sequenced within two weeks, and since then, scientists around the world have been working tirelessly to develop the vaccine that will bring the pandemic to an end. The early results from the vaccine developed here at the University of Oxford are promising.
Our best strategy in the age-old fight against germs is our collaborative, data-based effort to study the world around us and within us. Our best strategy is science.
Continue reading on Our World in Data:
Our data and research on the COVID-19 pandemic
We currently focus our efforts on the data and research on the COVID-19 pandemic. What does the latest data say? How can we win the battle against COVID-19?
Endnotes
An excellent book is Dorothy H. Crawford’s Deadly Companions: How Microbes Shaped our History (2009).
See the time-series of the English population here.
Mortality was similarly high, or even higher, in other parts of Europe.
In his history of the Black Death, Ole Jørgen Benedictow suggests that 60% of the population of Europe died in that pandemic. [See Benedictow (2004) – The Black Death 1346–1353: The Complete History.]
See Noble David Cook (1998) – Born to Die: Disease and New World Conquest, 1492-1650. Cambridge University Press.
See the archive of Moxon here moxforum.co.uk/archive/
Shaw‐Taylor, L. (2020). An introduction to the history of infectious diseases, epidemics, and the early phases of the long-run decline in mortality. The Economic History Review, 73(3), E1–E19. https://doi.org/10.1111/ehr.13019
D. A. Henderson (2009) – Smallpox: The Death of a Disease - The Inside Story of Eradicating a Worldwide Killer. Published by Prometheus Books.
The Wikipedia entry on smallpox includes several photos of smallpox survivors. On Google, you find more.
Shaw‐Taylor, L. (2020). An introduction to the history of infectious diseases, epidemics, and the early phases of the long-run decline in mortality†. The Economic History Review, 73(3), E1–E19. https://doi.org/10.1111/ehr.13019
Richard Carter (1966) – Breakthrough: The Saga of Jonas Salk. Trident Press.
The latest statistics on polio cases globally can always be found at polioeradication.org/polio-today/polio-now/this-week
WHO (2019) – Measles, Key Facts. 5 December 2019. Online here https://www.who.int/en/news-room/fact-sheets/detail/measles
Guerra, F. M., Bolotin, S., Lim, G., Heffernan, J., Deeks, S. L., Li, Y., & Crowcroft, N. S. (2017). The basic reproduction number (R0) of measles: A systematic review. The Lancet Infectious Diseases, 17(12), e420–e428. https://doi.org/10.1016/S1473-3099(17)30307-9
Cholera, Dengue fever, Diphtheria, Haemophilus influenzae type b, Hepatitis A, Hepatitis B, Hepatitis E, Human papilloma-virus, Influenza, Japanese encephalitis, Malaria, Measles, Meningococcal disease, Mumps, Pneumococcal disease, Pertussis, Poliomyelitis, Rabies, Rotavirus gastroenteritis, Rubella, Tetanus, Tick-borne encephalitis, Tuberculosis, Typhoid fever, Varicella, Yellow fever, Shingles (Herpes Zoster), and Smallpox. See https://en.wikipedia.org/wiki/Vaccine-preventable_diseases and https://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/
Cite this work
Our articles and data visualizations rely on work from many different people and organizations. When citing this article, please also cite the underlying data sources. This article can be cited as:
Max Roser (2020) - “Our history is a battle against the microbes: we lost terribly before science, public health, and vaccines allowed us to protect ourselves” Published online at OurWorldInData.org. Retrieved from: 'https://ourworldindata.org/microbes-battle-science-vaccines' [Online Resource]BibTeX citation
@article{owid-microbes-battle-science-vaccines,
author = {Max Roser},
title = {Our history is a battle against the microbes: we lost terribly before science, public health, and vaccines allowed us to protect ourselves},
journal = {Our World in Data},
year = {2020},
note = {https://ourworldindata.org/microbes-battle-science-vaccines}
}Reuse this work freely
All visualizations, data, and code produced by Our World in Data are completely open access under the Creative Commons BY license. You have the permission to use, distribute, and reproduce these in any medium, provided the source and authors are credited.
The data produced by third parties and made available by Our World in Data is subject to the license terms from the original third-party authors. We will always indicate the original source of the data in our documentation, so you should always check the license of any such third-party data before use and redistribution.
All of our charts can be embedded in any site.